Author Explains why Heroin Users Need Their Pot
By Richard Adamski
I started smoking cannabis when I was aged 19 and smoked it for about thirty years. For a period of about two years I took methamphetamine, originally ‘bombing’ it (putting the powdered drug tightly in a small piece of tissue or a rolling paper and swallowing it). I progressed to injecting methamphetamine and became addicted to it for about 8 months. At the time I was self-employed and could afford both drugs, namely meth and cannabis. It was when I got off methamphetamine that I started writing about drugs, particularly cannabis. I was still smoking cannabis then. To be honest the only reason I eventually stopped smoking cannabis and cigarettes is because I was diagnosed with COPD (chronic obstructive pulmonary disease). Years of smoking both drugs caused my COPD.
Over the years I got to know and mixed with a lot of drug users and I asked them all the same question: ‘What was the first drug you took?’ and every reply was cannabis and they continued to smoke it while they took harder drugs. Without question, cannabis is the introductory drug to other drugs. Most drug users start with cannabis. No one has died from smoking cannabis but indirectly they have. I personally know four people who have died because of a heroin overdose and the first drug they took, and continued to take up to their deaths, was cannabis.
Why Cannabis Fits so Well with Class A Drugs
Cannabis goes well with Class A drugs, i.e. heroin and methamphetamine. For example: If you have a toot (burn off the foil) of heroin, then inhale cannabis, keep the smoke in your body for several seconds then exhale, the cannabis increases the heroin effect. Cannabis goes well while you’re buzzing on methamphetamine. Like heroin, when you come down off the drug, a cannabis joint lessens the withdrawal effect.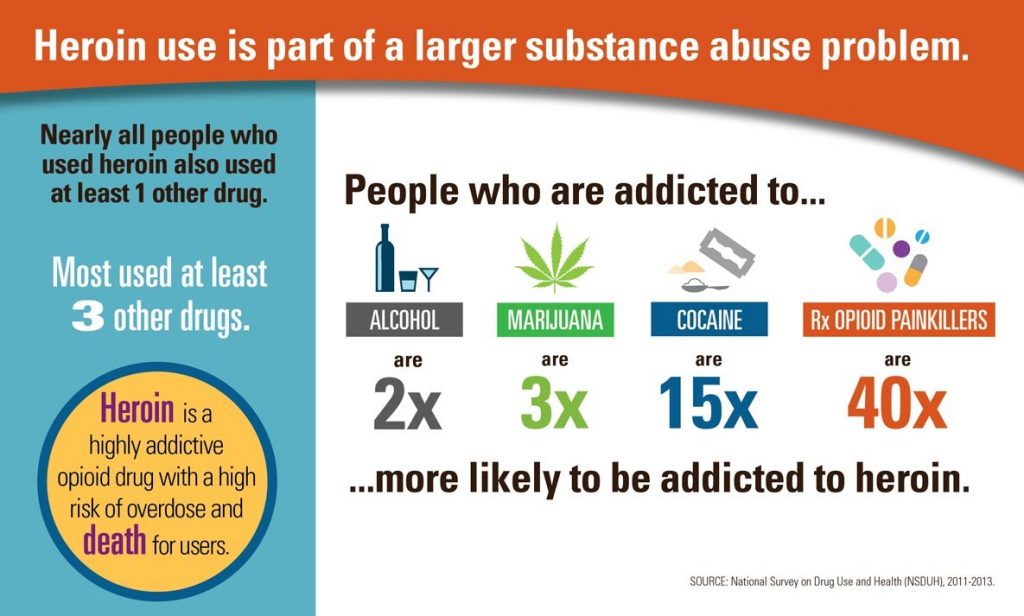
The side effects of excessive use of cannabis range from anxiety and paranoia to problems with attention, memory and coordination and while you continue to smoke cannabis you are keeping the illegal drug industry going. Cannabis and Class A drugs undeniably go together like peaches and cream. The only people who need cannabis are those who smoke it.
Some people may say that I’m a hypocrite in writing what I have done as I took drugs over a long period of time. All I can say in my defense is that with taking drugs and mixing with and meeting drug users, I have seen how cannabis runs the drug show.
What about marijuana used as medicine?
There’s massive support for cannabis to be decriminalized or legalized and a lot of famous people support this action. In the UK the BMA (British Medical Association) voted overwhelmingly for cannabis to be made available for such as cancer and MS sufferers. A while ago there was a big national debate about cannabis and in one of the national newspapers there was a half-page photograph of an elderly MS sufferer with a cannabis joint in his mouth. To me that is setting a bad and dangerous example. ‘If he can smoke it, then why can’t I?’ and ‘It’s not doing him any harm so why should it me?’
If such as the MS sufferer could be medically supplied with cannabis in such as a tincture way (dissolved in alcohol), cake, organic yoghurt, as a pill and only available on prescription then that would shut him up and others like him of a similar persuasion. In my opinion cannabis should never be made legal in herbal, grass, weed, because it is in this form where the cannabis problems lie.
Broken Dreams and Death: Marijuana at 14, then heroin
I knew a young man named Ross who dealt cannabis and injected heroin. He didn’t deal heroin. He wasn’t an addict and took heroin and cannabis as recreational drugs. He died at the age off 22 because he had a bad hit of heroin. Whether it was cut with a bad substance I don’t know, but he was found dead in his flat with the needle still in his arm. Ross once told me: ‘I actually wanted to be a pilot in the RAF (Royal Air Force), but at the age of 14 I started smoking Ganga and that put an end to that.’
In my strong opinion, cannabis is the most dangerous drug because most people think it isn’t.
Richard Adamski is the author of Three Trees. Three Trees is a contemporary Wind in the Willows where woodland creatures act as humans do in the environment they live in. An anti-drug theme runs throughout the story. He lives in England.